National Screening Survey
Overview
The American Cancer Society Cancer Action Network (ACS CAN) empowers advocates across the country to make their voices heard and influence evidence-based public policy change, as well as legislative and regulatory solutions to reduce the cancer burden. As part of this effort, ACS CAN deploys surveys to better understand cancer patient and survivor experiences and perspectives, through our Survivor Views research panel. This special project expands the survey audience beyond cancer patients and survivors to include the national adult screening population age 45 and over.
This survey explores experiences with routine cancer screening among the general population as well as experiences after a cancer diagnosis. The web-based screening population survey was conducted April 25-28, 2025, among 1,000n adults age 45+ nationwide. Where appropriate, results are combined with those of ACS CAN’s Survivor Views cohort of cancer patients and survivors, from a web survey conducted March 24-April 16, 2025. Full methodological detail is provided at the end of this document.
Key Findings
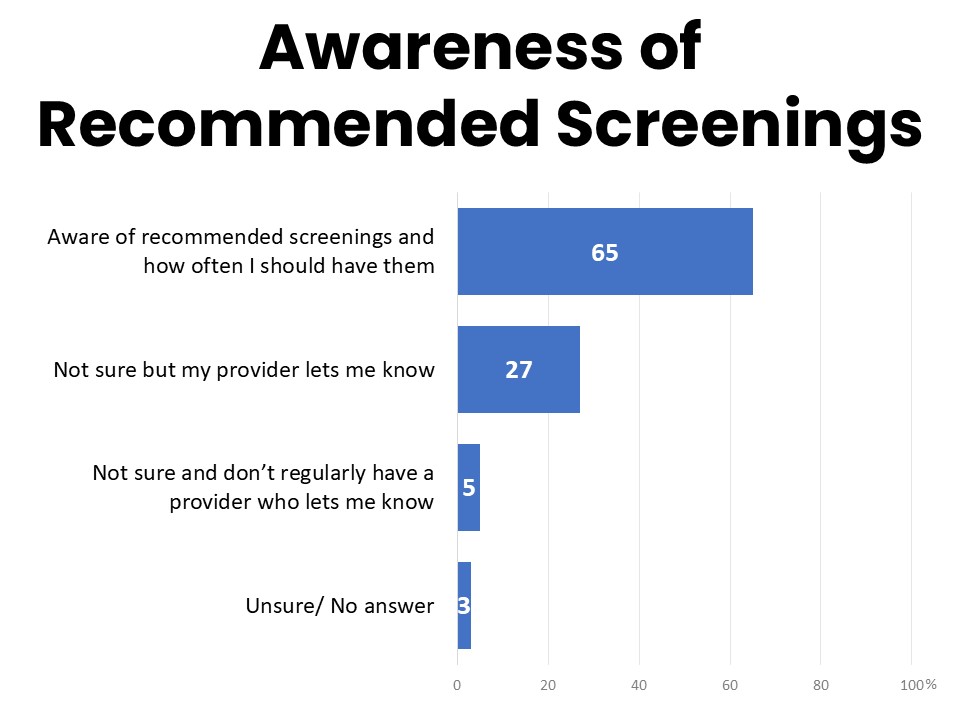
- Two-thirds (65%) are aware of their recommended routine cancer screenings and how often to have them, while others rely on their provider to let them know
- 31% report being more than a year behind on a recommended routine cancer screening. The single most frequently mentioned reason for falling behind is concerns about costs (14%)
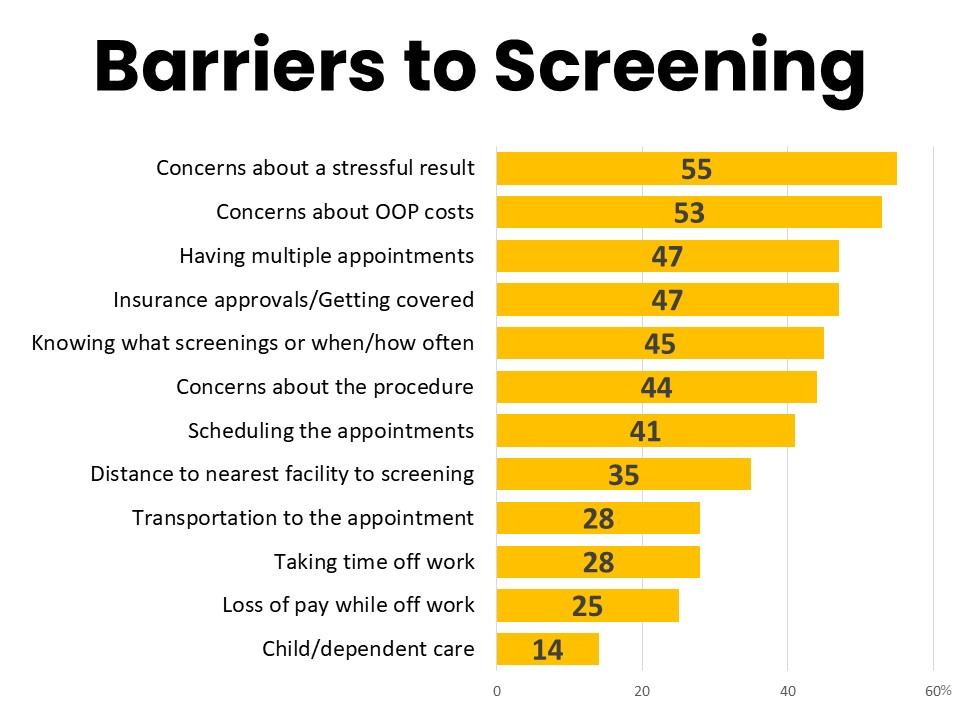
- The survey identified several other barriers to screening including insurance pre-approvals (47%), having to schedule multiple appointments (47%), and knowing what screenings to have and when to have them (45%), but concerns about out-of-pocket costs top all of these (53%)
- 18% have received a bill for a routine screening and 22% of those who required follow-up testing received a bill for the follow-up
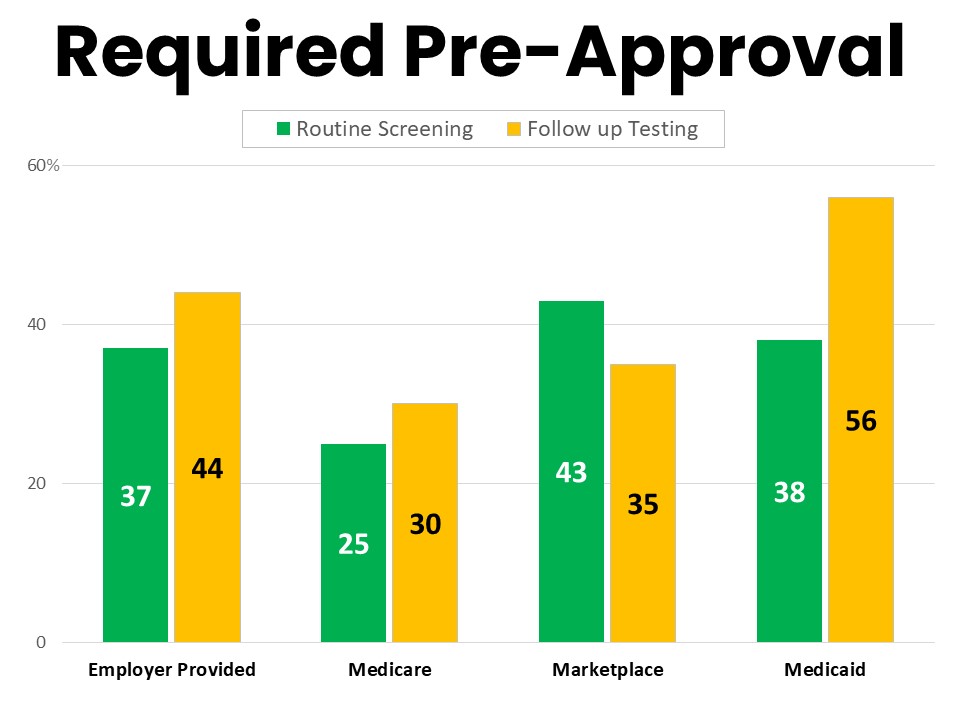
- 31% have had to get approval from their insurance before scheduling a routine screening and 40% of those said it took two weeks or more to get the approval
- Patients report high satisfaction with post-screening communication of results from their providers
- Majorities say they have not received assistance from their provider’s office with many screening-related tasks
Detailed Survey Findings
Two Thirds are Aware of Screening Eligibility and Frequency But Many Rely on Providers' Guidance
Sixty-five percent of those surveyed say they are aware of the routine cancer screenings that are recommended for them and how often they should have them. Another 27% say they are not always sure but their provider lets them know when it’s time, while 5% say they aren’t sure and don’t regularly have a provider who lets them know when it’s time for a screening.
Those with employer-provided health plans and Medicare enrollees are significantly more likely to say they know what their recommended screenings are and when to get them (69% and 68% respectively) than those with Marketplace plans (55%) or those with Medicaid as their primary coverage (51%). Women are also significantly more likely to report knowing what screenings they are eligible for and when to have them (68%) than men (60%), and those in higher income households are also more likely to be knowledgeable about their recommended screenings than those in lower income households (69% of those earning over $125k annually compared to 55% of those in households earning less than $55k per year).
Ninety-four percent of respondents report having a primary care doctor, and 93% say they typically see a primary care doctor at least once per year. Ninety-one percent have seen a primary care doctor within the past twelve months while just 9% have not. Over one-third (35%) say they have not had a routine cancer screening in the past twelve months.
Thirty-One Percent Have Been Behind on Recommended Screenings by More Than One Year
Nearly a third of screening age adults (31%) report having been more than a year behind on recommended cancer screenings, while 55% say they have not and another 13% are unsure. Medicaid recipients (41%) and those with privately-purchased marketplace plans (39%) are significantly more likely that Medicare enrollees (27%) and those with employer-provided plans (31%) to have fallen behind on recommended screenings.
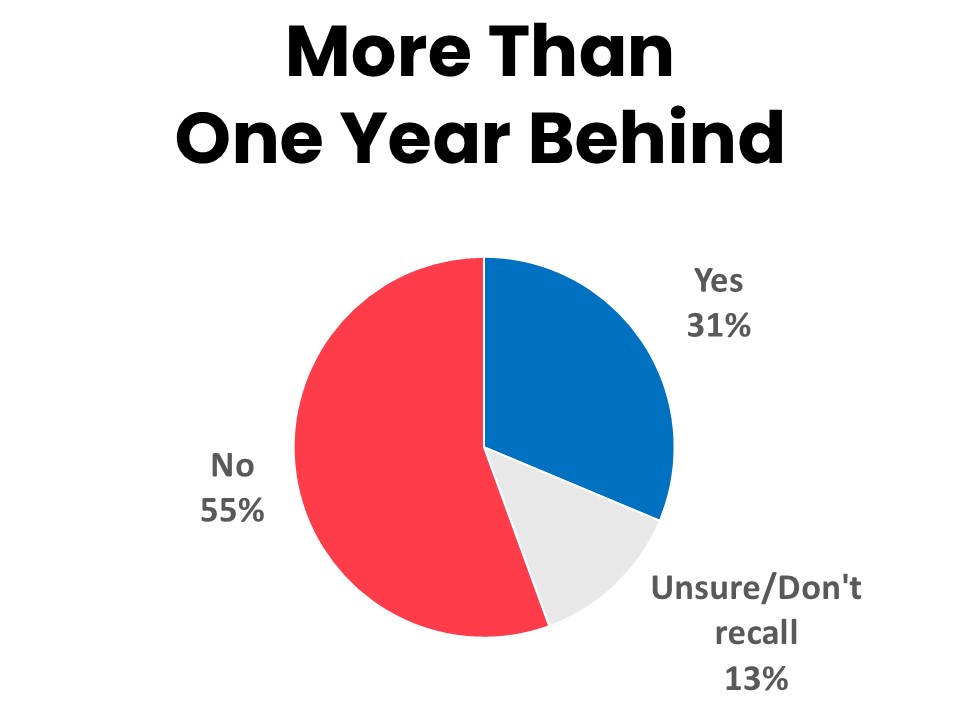
Women (40%) are much more likely than men (23%) to report falling a year or more behind on recommended screenings, while men are twice as likely as women to say they don’t know (16% vs. 9%). Those in higher income households are less likely to have fallen behind (25%) than those in lower income households (38%), and respondents in rural areas (39%) are also more likely than those in urban settings (29%) to have fallen behind by more than a year. Sixty-one percent of those who do not have a regular primary care doctor report having been more than a year behind on their recommended screenings.
Cost is the Single Most Frequently Mentioned Reason for Falling Behind
When asked the main reason for being behind on routine cancer screenings, the single most frequently mentioned response was cost concerns/not being able to afford it, mentioned by 14%. Among those on privately-purchased marketplace plans, one-in-five said cost was the main reason for falling behind. By comparison, the next most frequently mentioned reasons are a lack of concern about cancer risk (10%), not having enough time (9%), having forgotten an appointment (9%), and scheduling difficulties and long wait times (8%).
Asked to rate a list of potential barriers, concerns about out-of-pocket costs (53%) topped over significant barriers including having to schedule multiple appointments (47%), insurance approvals (47%), and knowing what screenings to have and when to have them (45%). The only item tested that is more concerning that worries about costs is concerns about getting a bad result (55%). Medicare enrollees are significantly less likely than others to consider insurance approvals a barrier to screening (39%), while those enrolled in privately-purchased marketplace plans are most likely to feel getting the screening covered is a barrier (58%).
While worries about affordability present a significant barrier to screening, the cost of screening should typically be covered by insurance. However, 18% say they have received a bill for a routine cancer screening and 22% of those who required follow-up testing received a bill for the follow up. Medicare enrollees are significantly less likely to report receiving a bill for a routine screening (14%), while those with employer-provided plans are most likely (23%). Sixteen percent recall receiving a bill for a preventive service that should have been covered and having the bill changed or forgiven.
In addition to the national screening age survey population, the ACS CAN Survivor Views cohort of 1,246 cancer patient and survivors diagnosed or treated within the past seven years also answered questions about their experiences with cancer screening. Among cohort members who were diagnosed with cancer following a routine screening, 49% report that they received a bill for additional screening they required after their initial abnormal result. Eighty-six percent of cancer patients and survivors surveyed report that they have continued to receive routine screenings for cancers other than the cancer they were diagnosed with, and 41% of those have received a bill for these screenings.
Three-in-Ten Have Required Insurance Pre-Approval for Routine Cancer Screenings
Nearly one-third (31%) have had to get approval from their insurance before scheduling a routine screening and 40% of those said it took two weeks or more to get the approval. Among those who required follow-up testing after a routine cancer screening produced an unclear or concerning result, 37% were required to get insurance pre-approval in order to get the follow up testing. This adds additional delays, with 27% saying it took five days or more to get that pre-approval before the follow-up could be scheduled. Medicaid subscribers are much more likely to report needing pre-approval for follow-up testing (56%), while Medicare enrollees are the least likely group (30%).
Patients Report High Satisfaction with Post-Screening Communication with Providers, but Many Do Not Receive Assistance with Screening Tasks
When a routine cancer screening result is normal, the most common way patients report being notified is online via email or patient portal notification from their provider (31%), followed by a phone call from the provider’s office (26%). Fourteen percent learn their result in a follow-up appointment, while 12% receive an email or portal notification from the testing facility and another 12% are notified via US mail. Ninety-six percent say they are satisfied with the amount of information they receive and their ability to ask any questions of their provider.
Among those who have received an abnormal result from a routine cancer screening, 60% are notified via a phone call from the provider’s office, and 19% learn their result in a follow up appointment. Significantly fewer (13%) were first notified of an abnormal result in an email or portal notification from their provider compared to those who received a normal result that way, and just 4% discovered their abnormal result in an email or digital notification from a testing facility. Another 4% received the information via US mail. While 90% agree they received all the information they needed to understand their result and next steps and were able to ask any questions they had, only 55% strongly agree with this statement. Over one-third (35%) agree only somewhat, while 8% disagree.
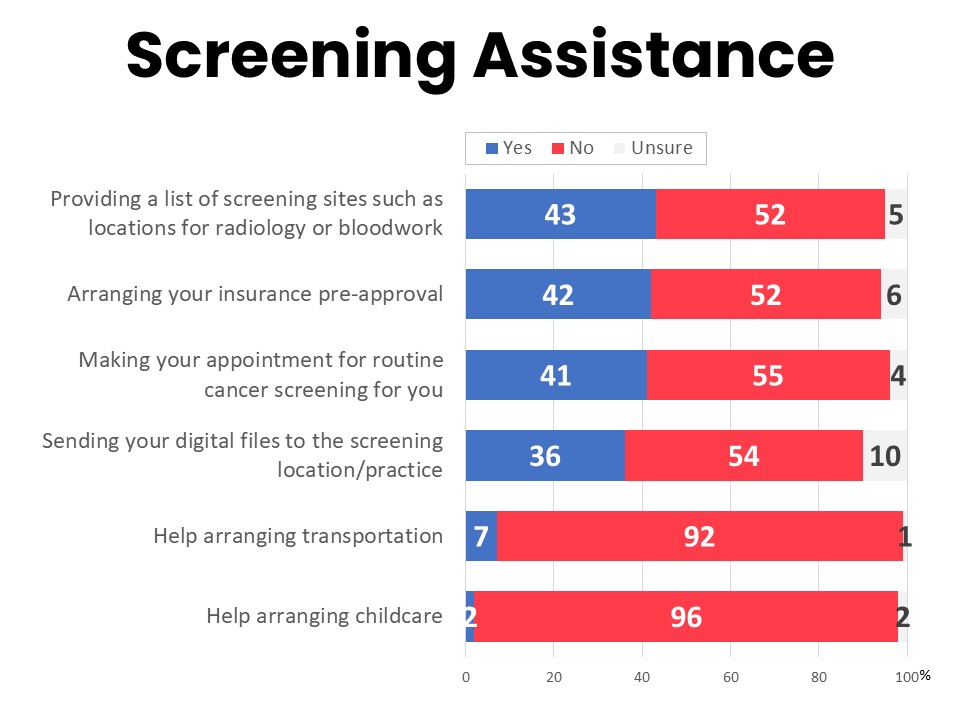
Majorities of patients report that they are not receiving assistance from their provider’s office with many key tasks related to cancer screenings. While 43% say their provider’s office has provided a list of screening sites such as locations for radiology or bloodwork, 52% have not been offered this. Forty-two percent report receiving help with insurance pre-approvals, while 52% say they have not. Forty-one percent say their provider’s office has made their appointment for routine screening for them while 55% have not had a provider make the appointment. While 36% say their provider has helped by sending digital files to the screening location, 54% say their provider has not done this, although 10% are unsure. Just 7% have had help arranging transportation and 2% have had a provider’s office assist with arranging childcare.
Methodology
The National Screening Survey data was collected online April 25-28, 2025 among 1,000 screening age adults nationwide (age 45+), with demographic and regional distribution proportionate to the population. Differences reported between groups are tested for statistical significance at a 95% confidence interval.
ACS CAN’s Survivor Views research initiative was designed to support the organization’s efforts to end suffering and death from cancer through public policy advocacy. Data provided by cancer patients and survivors as part of this project allows for a greater understanding of their experiences and opinions on cancer-related issues and gives voice to cancer patients and survivors in the shaping and advocating of public policies that help prevent, detect, and treat cancer and promote a more positive quality of life for those impacted.
To ensure the protection of all participants in this initiative all research protocols and operations are reviewed by the Morehouse School of Medicine Institutional Review Board.
The survey population is comprised of individuals who meet the following criteria:
- Diagnosed with and/or treated for cancer within the last seven years
- Over the age of 18 (parents of childhood cancer survivors were invited to participate on behalf of their minor children)
- Reside in the US or US territories
Survivor Views participants are invited to participate through email, direct mail, social media, and outreach to communities and partners engaged with cancer patients and survivors. Those who agree to participate after reviewing the informed consent information are invited to join the Survivor View’s research cohort and participate in future surveys. This survey also includes cancer patients and survivors nationwide from probability and non-probability panels. The data for this survey were collected between March 24-April 16, 2025. A total of 1,246 participants responded to the survey.
About ACS CAN
The American Cancer Society Cancer Action Network (ACS CAN) advocates for evidence-based public policies to reduce the cancer burden for everyone. We engage our volunteers across the country to make their voices heard by policymakers at every level of government. We believe everyone should have a fair and just opportunity to prevent, detect, treat, and survive cancer. Since 2001, as the American Cancer Society’s nonprofit, nonpartisan advocacy affiliate, ACS CAN has successfully advocated for billions of dollars in cancer research funding, expanded access to quality affordable health care, and advanced proven tobacco control measures. We stand with our volunteers, working to make cancer a top priority for policymakers in cities, states and our nation’s capital. Join the fight by visiting www.fightcancer.org.