Survivor Views: Surprise Billing and Prescription Cost and Coverage Survey Findings Summary
Overview:
The American Cancer Society Cancer Action Network (ACS CAN) established Survivor Views in January 2019. The project has established a cohort of 3,055 cancer patients and survivors diagnosed with and/or treated for cancer within the last five years who are willing to share their opinions and experiences through a series of surveys focused on policy issues impacting cancer patients and survivors.
In October 2019, Survivor Views conducted a cohort survey focused on their experiences accessing and paying for cancer care, including the cost of prescription drugs and their experiences receiving surprise bills. One thousand three hundred and ninety-two cohort members responded to the web-based survey (a 46% response rate). This sample provides a margin of error +/- 3% and 97% confidence level. The research provides important insights into the experiences of cancer patients and survivors in accessing and affording health care and medication to treat their cancer or prevent it from returning.
Key Findings:
Key findings from the survey include:
- Nearly one-third (30%) of cancer patients and survivors have experienced at least one insurance-related barrier to accessing their prescribed medication, including delays while waiting for additional insurance approvals, lack of coverage for the prescribed drug, and being required to try a less expensive drug first (also known as step therapy). Seventy-nine percent of respondents who reported a barrier experienced negative health or lifestyle consequences, including additional time spent resolving the issue, additional expense to obtain the drug, or difficulty controlling pain or declines in overall health due to the delay.
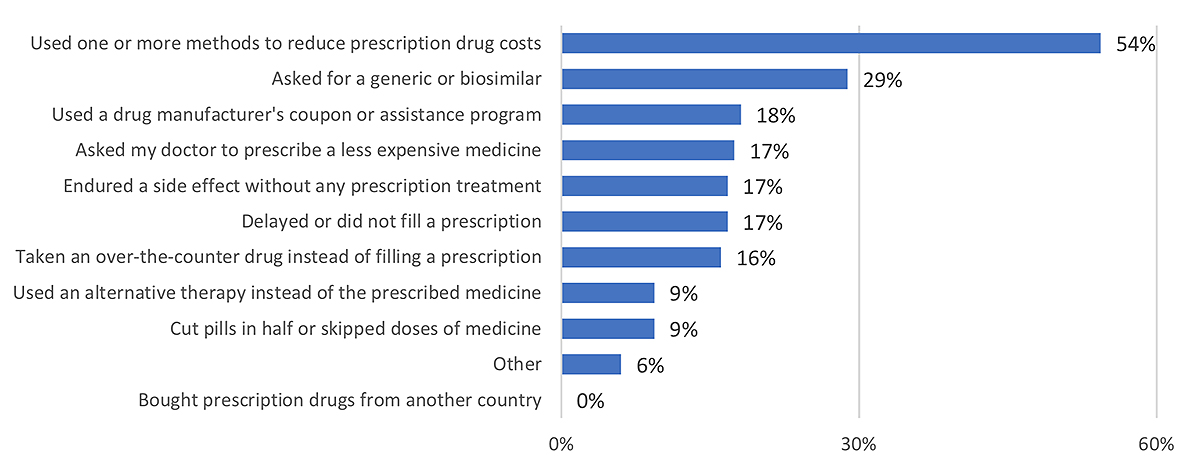
- Lower income cancer patients are more likely to report difficulty affording prescription drugs and more likely to have experienced barriers filling prescriptions (41%). Perhaps in response to these challenges, more than half (54%) of cancer patients and survivors earning $30,000 or less have acted to reduce their out-of-pocket costs. Some methods may be not harmful, such as asking for a generic or biosimilar or using a manufacturer’s coupon. However, other common methods used disproportionately by lower income respondents may have serious negative health effects, such as delaying or not filling prescriptions, skipping doses, or cutting pills in half.
- Nearly a quarter (24%) of survey respondents have received a surprise medical bill. Surprise bills may occur when patients receive unexpected bills and may occur when a patient unknowingly receives services from an out-of-network provider (for example, when being treated at an in-network hospital) or is treated at an out-of-network facility during a medical emergency. Sixtyone percent of the surprise bills were for over $500, and 21% were $3,000 or more. Receiving surprise bills negatively impacted respondents’ behavior, making them more likely to experience anxiety about receiving another surprise bill or paying for treatment, less likely to follow up with a recommended specialist who may be out of network, and less likely to call an ambulance or visit the emergency room when experiencing a serious health issue related to their cancer.
Detailed Survey Findings
The survey asked cancer patients and survivors about the cost and perceived affordability of prescription drugs they are taking for their cancer. Nearly two-thirds (63%) of all respondents are currently taking one or more prescription drugs; among those currently in treatment, this figure
increases to 84%. While 64% of respondents spend less than $50 per month on their current prescriptions, as this amount increases, so does the difficulty in affording the expense. Indeed, 58% of respondents who are spending more than $100 per month on their prescriptions report that this cost is difficult or very difficult to afford.
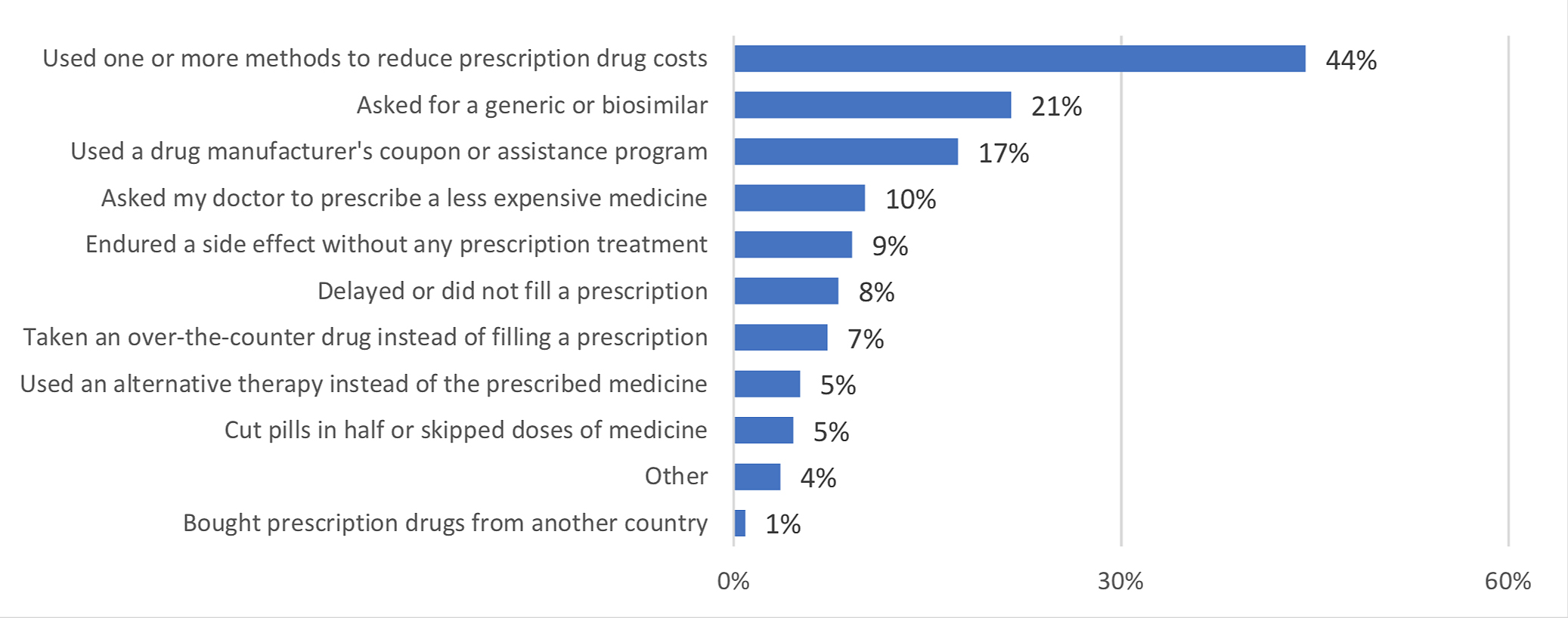
In efforts to lower their prescription drug expenses, 44% of cancer patients and survivors are employing a range of cost-reduction methods. Some of the common methods may help lower the cost of their care without impacting their health, such as asking for a generic or bio-similar (22%), using a drug manufacturer’s coupon or assistance program (17%), or asking their doctor to prescribe a less expensive medicine (10%). However, other methods may be less benign, such as forgoing medication for a cancer side effect (9%), delaying or not filling a prescription (8%), or attempting to ration medication or reduce use (5%).
Figure 1: Actions taken to reduce cost of prescription drugs; all respondents
These findings raise concern about the affordability of prescription drugs for all cancer patients and survivors. However, the results show that lower-income respondents are particularly impacted by challenges paying for prescribed medications. They are more likely to have undertaken nearly all methods of cost containment when compared to their higher income counterparts. In an effort to reduce prescription drug costs, lower income respondents are more likely to endure cancer side effects without treatment, more likely to delay or not fill a prescription, and more likely to cut pills in half or skip doses.
Figure 2: Actions taken to reduce cost of prescription drugs; annual household income <$30,000
Thirty percent of survey respondents also reported having experienced one or more challenges in insurance payments for their prescription drugs. These barriers include the need to wait more than 24 hours for additional insurance approvals (19%), lack of coverage for a prescribed drug (14%), and requirements to try a less expensive drug before getting the one prescribed by their doctor (10%).
After encountering a barrier, 80% of respondents suffered negative consequences such as having to spend significant time on the phone with the insurer to resolve the issue or paying for the drug out of pocket. Time and expense are not insignificant challenges for cancer patients to endure. However, perhaps more concerning are the health consequences of these challenges, which included inability to control cancer pain, delays in the treatment plan, declining health. Six percent of cancer patients or survivors who encountered one of these insurance barriers were never able to obtain the prescribed medication.
The survey also asked cancer patients and survivors to share their experiences receiving a surprise bill. Surprise bills may occur when patients receive unexpected bills and may occur when a patient unknowingly receives services from an out-of-network provider (for example, when being treated at an in-network hospital) or is treated at an out-of-network facility during a medical emergency. Nearly a quarter of respondents indicate they have received a surprise bill for their cancer care.
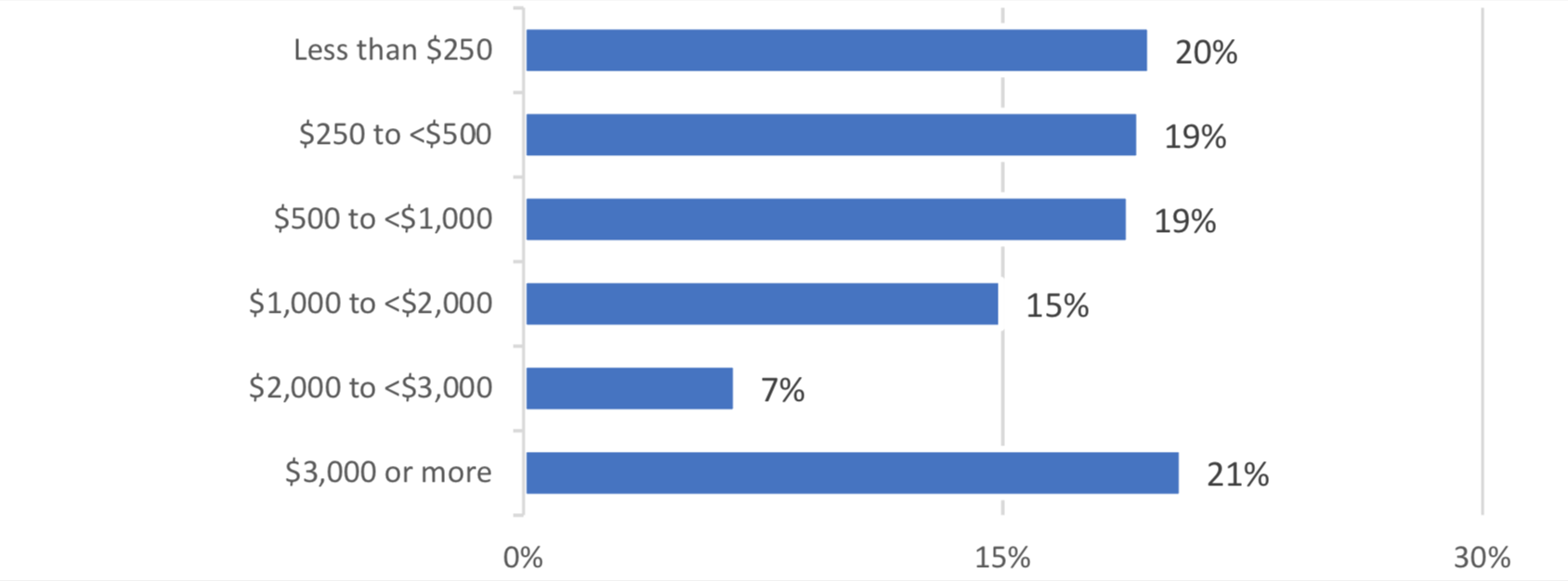
In the majority of cases, surprise bills are not an insignificant expense. Sixty-one percent of the surprise bills received by survey respondents were for more than $500, 43% were more than $1,000, and 21% were over $3,000. The Federal Reserve reports four in ten Americans cannot afford an unexpected bill of $400 or more,1 highlighting the serious impact of these bills on the financial stability of cancer patients and survivors.
Figure 3: Dollar amount of surprise bills received by cancer patients and survivors
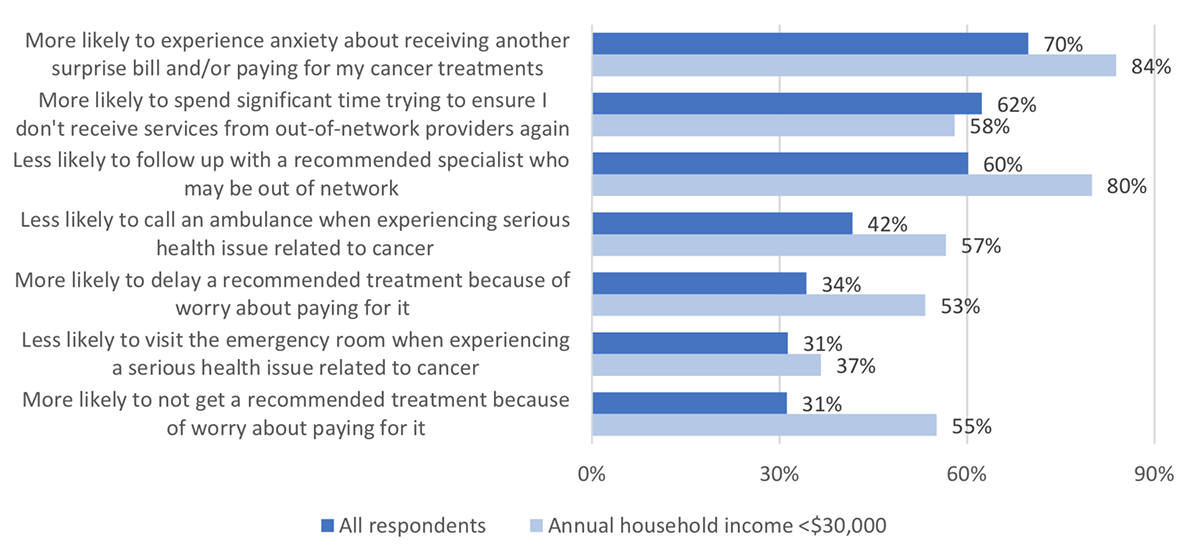
The experience of receiving a surprise bill has negative behavioral consequences for future health decisions made by cancer patients and survivors. Survey respondents who received a surprise bill reported that as a result of the experience they are more likely to experience anxiety about receiving another surprise bill or paying for their cancer treatment (70%), less likely to follow up with a recommended specialist who may be out of network (60%) and less likely to call an ambulance (42%) or visit the emergency room (31%) when experiencing a serious health issue related to their cancer.
Once again, these impacts are more severe among lower income cancer patients and survivors. Compared to higher income individuals, respondents with annual household income below $30,000 reported a higher incidence of every negative behavioral impact tested except spending significant time on the phone or in the doctor’s office trying to ensure they do not receive services from an out-of- network provider again. The magnitude of this difference was greatest for:
- More likely to not get a treatment recommended by their doctor because they are worried about paying for it (55%, compared to 31% for all respondents)
- More likely to delay a treatment recommended by their doctor because they are worried about paying for it (53%, compared to 34% for all respondents)
- Less likely to follow up with a specialist recommended by their doctor who may be out of network (80%, compared to 60% for all respondents)
Figure 4: Behavioral impact of receiving a surprise bill on cancer patients and survivors
Overall, the Survivor Views surprise billing and prescription drug coverage results demonstrate some of the serious challenges faced by cancer patients and survivors in paying for their cancer care. Their impact has negative consequences for the health and behaviors of individuals in the future, and present particularly concerning challenges for lower income patients and survivors.
The next Survivor Views survey, covering topics related to patient data, genetics, and privacy, is currently in the field through mid-December 2019.
Methodology
Survivor Views is an ACS CAN initiative designed to enhance the organization’s mission to end suffering and death from cancer. Data provided by cancer patients and survivors as part of this project allows for a greater understanding of their experiences and opinions on cancer-related issues and gives voice to cancer patients and survivors in the shaping and advocating of public policies that help prevent, detect, and treat cancer and promote a more positive quality of life for those impacted.
To ensure the protection of cohort participants as we pursue these objectives, all research protocols, questionnaires, and communications undergo review by the Morehouse School of Medicine Institutional Review Board.
The Survivor Views cohort is comprised of individuals who meet the following criteria:
- Diagnosed with and/or treated for cancer within the last five years
- Over the age of 18
- Reside in the US or US territories
This survey was conducted using a web-based survey sent to 3,007 Survivor Views cohort members. The data were collected between October 7 and October 30, 2019. A total of 1,392 participants responded to the survey, a 46% response rate. This sample provides a margin of error +/- 3% and 97% confidence level.
About ACS CAN
The American Cancer Society Cancer Action Network (ACS CAN) is making cancer a top priority for public officials and candidates at the federal, state and local levels. ACS CAN empowers advocates across the country to make their voices heard and influence evidence-based public policy change as well as legislative and regulatory solutions that will reduce the cancer burden. As the American Cancer Society’s nonprofit, nonpartisan advocacy affiliate, ACS CAN is critical to the fight for a world without cancer. For more information, visit www.fightcancer.org.
1 https://www.federalreserve.gov/publications/2019-economic-well-being-of-...