Survivor Views: Majority Less Likely to Get Recommended Screenings if Coverage is Lost
Overview
The American Cancer Society Cancer Action Network (ACS CAN) empowers advocates across the country to make their voices heard and influence evidence-based public policy change, as well as legislative and regulatory solutions that will reduce the cancer burden. As part of this effort, ACS CAN deploys surveys to better understand cancer patient and survivor experiences and perspectives, through our Survivor Views research panel. The panel is a group of cancer patients and survivors who respond to regular surveys and provide important insights to support ACS CAN’s advocacy work at all levels of government.
Fielded April 2-20, 2023, our latest survey explores cancer patients’ and survivors’ experiences related to receiving preventive health care, the adequacy of coverage networks, and the need for patient navigators. The web-based survey was conducted among 1,311 patients and survivors nationwide who have been diagnosed with or treated for cancer in the last seven years.
Key Findings
-
A majority (58%) of cancer patients and survivors say they would be less likely to stay up to date with preventive care if the provision mandating 100% coverage was repealed, resulting in a patient out-of-pocket cost for these services. Fifty-three percent put the dollar amount that would present a barrier to accessing preventive services at less than $200. For 28%, it is under $100.
-
Twelve percent of cancer patients and survivors have at some point not been able to get the care they needed in-network, and 34% have received out-of-network care (often because the out-of-network provider had more relevant expertise than their in-network option). When using out-of-network care, it is most often sought for treatments including chemotherapy and radiation (21%), specialty services (21%), surgical or hospital care (15%), and for lab services (13%).
- Of the 34% who have received out-of-network care, 23% say the cost was not covered at all, and 25% did not know in advance that there would be additional costs for the out-of-network care. Twenty-three percent report delaying care because they were unable to find an in-network provider, and 8% report not seeking the care at all.
- Fifty-five percent say their primary oncology provider has a patient navigator available on staff, while 35% are unsure.
- Nearly all (91%) agree it is important for cancer patients to have access to a patient navigator, and three-quarters (75%) say it is very important.
Detailed Survey Findings
A majority would be less likely to maintain preventive care, including recommended cancer screenings, if the mandate for full coverage is repealed
Under current regulations requiring that most plans cover recommended preventive services at no cost to patients, 86% of cancer patients and survivors surveyed say they don’t have difficulty getting the preventive services they need.
However, 58% say they would be less likely to stay current with their preventive services, which include recommended cancer screenings, if that provision were repealed resulting in a cost to patients for their preventive care. Just over one-quarter (26%) say they would be much less likely to stay current if there were a cost. Fifty-three percent put the dollar amount that would present a barrier to seeking preventive care at under $200. Over one-quarter (28%) say an amount under $100 would present a barrier.
Patients in lower income brackets would be even less likely to maintain their preventive care, including nearly three-quarters (72%) of the lowest income bracket surveyed, who earn under $35,000 in annual household income. Hispanic respondents are also at greater risk of falling short on preventive care without this coverage, with 75% saying they would be less likely to stay current and 45% much less likely.
Thirty percent have faced challenges related to network limitations
Thirty percent of respondents have faced challenges related to limitations with their provider network. The most frequently cited challenge (19%) is having to change providers due to a change in coverage, such as after a change in employer-provided insurance, meaning a patient’s care is no longer provided by the team most familiar with their oncology history.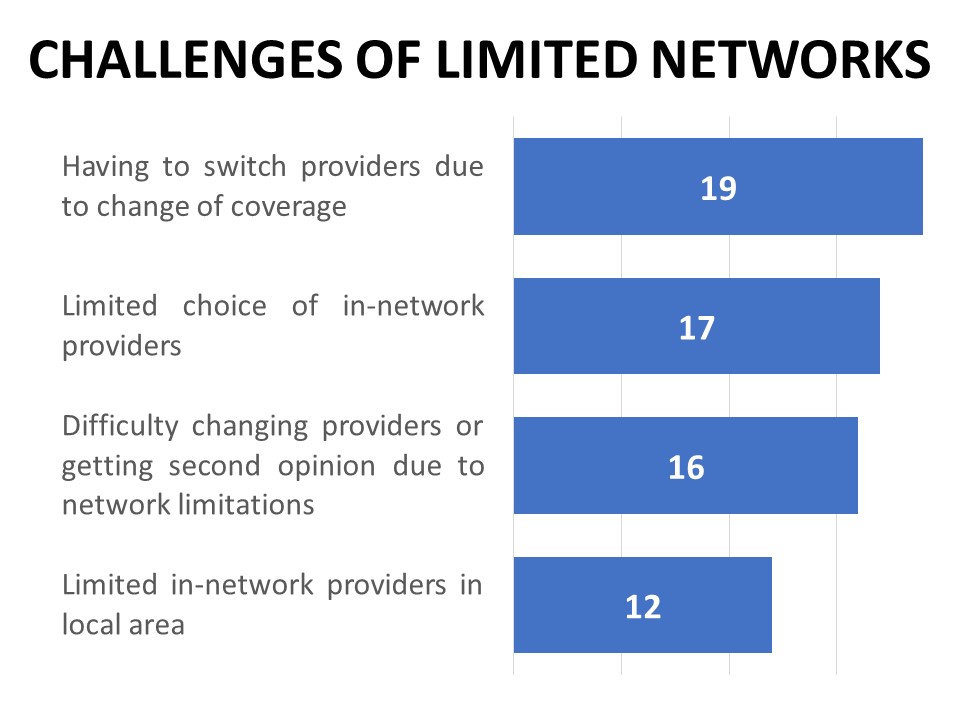
Other challenges related to network adequacy include a limited choice of in-network hospitals or treatment centers (17%), difficulty changing providers or seeking a second opinion due to limited choice of in-network providers (16%), or limited options for in-network providers in the local area (12%). Twelve percent of cancer patients and survivors have at some point not been able to get the care they needed in-network, including 13% of those on employer-provided plans and 15% of those purchasing their coverage privately such as through the marketplace.
One-third have received out-of-network care and 23% of those say it was not covered at all
Just over one-third (34%) have received out-of-network care, often because the out-of-network provider had more relevant expertise or a stronger recommendation than their in-network option (19%). Many report specific examples that illustrate the complexities of identifying providers, such as the following:
“Surgery was scheduled in-network without communicating the anesthesiologist is out of network, leaving me to reschedule the surgery once I found someone within my network. It wastes time for the patient, surgeon and anesthesiologist and costs money from missed appointments and loss of worktime, in addition to treatment delays for patient services that are needed to save lives.”
“The [out-of-network] plastic surgeon was the only one my in-network breast surgeon worked with. I also did not realize he was out of network and was actually told he was in my network.”
“My [employer-provided] insurance was not yet negotiated with my large surgical institution when I began treatment so I’m worried about facing difficulty having continued care with my current providers.”
“I was told by my plan provider that I had to travel for radiation treatment because the in-network facilities in my area didn’t have the right equipment. I needed treatment 5 days a week for 6 weeks and no hardship benefit was offered for the travel.”
Out-of-network care is most often sought for treatments including chemotherapy and radiation (21%), specialty services (21%), surgical or hospital care (15%), and lab services (13%). While 52% usually have a choice of multiple providers of a given service available within their plan, 12% typically do not (22% sometimes have a choice depending on the service).
Of the 34% who have received out-of-network care, 23% said the cost of that care was not covered at all, and 25% did not know in advance that there would be additional costs. In fact, 17% did not realize the provider was out of network before the visit. Nearly one-in-five (19%) have filed an appeal with their plan provider in order to get out-of-network care covered, and 45% of those were successful.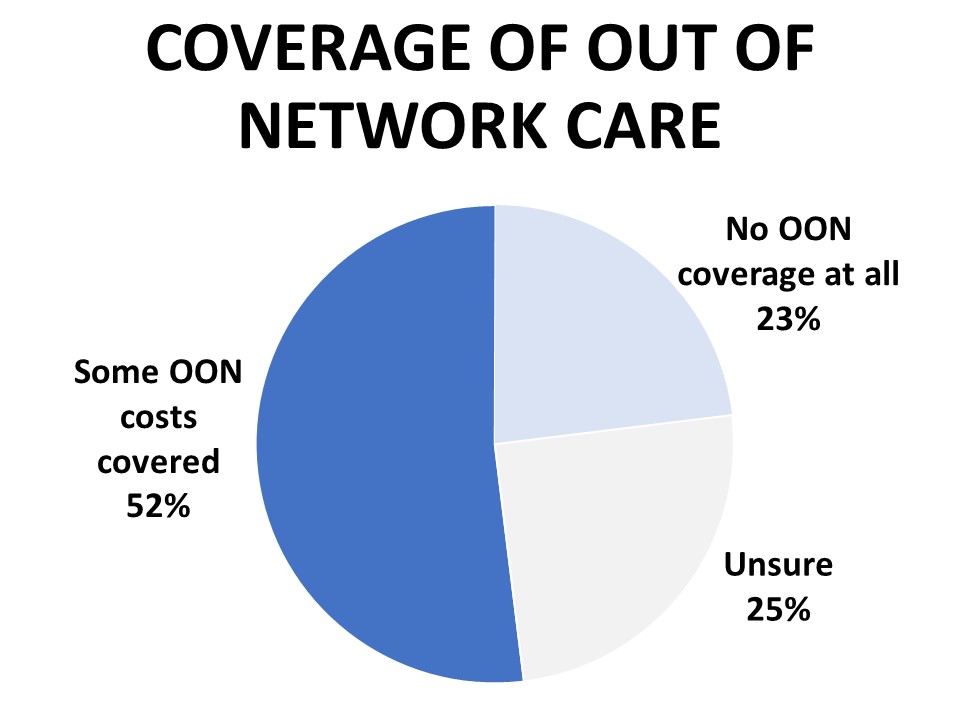
Twenty-three percent report delaying care because they were unable to find an in-network provider, and 8% report not seeking the care at all. Hispanic respondents are twice as likely as non-Hispanics to report delaying or not seeking care due to difficulty finding in-network providers (47%).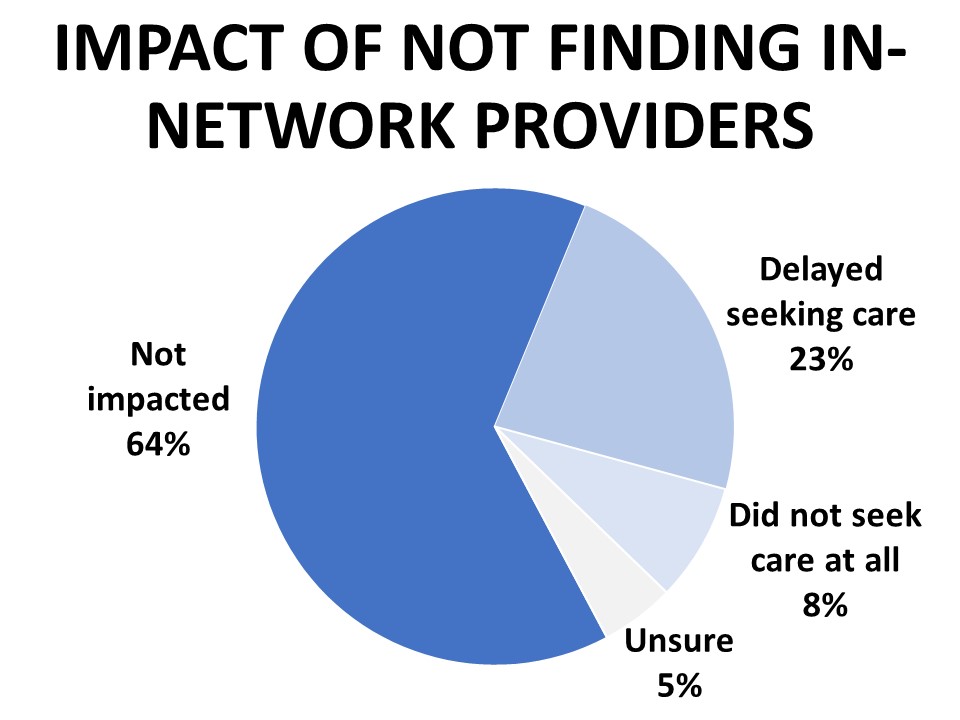
Nearly all agree it is important cancer patients have access to a patient navigator, but just 55% do
Fifty-five percent say their primary oncology provider has a patient navigator available on staff, while 35% are unsure. Nearly all (91%) agree it is important for cancer patients to have access to a patient navigator, and three-quarters (75%) say it is very important. Among those who have access to a patient navigator, the most widely cited benefit respondents mention is the time saved with help making appointments and gathering information. Twelve percent mention having a better understanding of their treatment options, followed by emotional support (9%), financial assistance (9%), and help finding specialists or other services (7%)
Methodology
ACS CAN’s Survivor Views research initiative was designed to support the organization’s efforts to end suffering and death from cancer through public policy advocacy. Data provided by cancer patients and survivors as part of this project allows for a greater understanding of their experiences and opinions on cancer-related issues and gives voice to cancer patients and survivors in the shaping and advocating of public policies that help prevent, detect, and treat cancer and promote a more positive quality of life for those impacted.
To ensure the protection of all participants in this initiative all research protocols, questionnaires, and communications are reviewed by the Morehouse School of Medicine Institutional Review Board.
The survey population is comprised of individuals who meet the following criteria:
- Diagnosed with and/or treated for cancer within the last seven years
- Over the age of 18 (parents of childhood cancer survivors were invited to participate on behalf of their minor children)
- Reside in the US or US territories
Potential Survivor Views participants were invited to participate through email invitations, social media promotion, and partner group outreach. Those who agreed to participate after reviewing the informed consent information completed a brief survey including demographic and cancer history information to inform analysis as well as topical questions as discussed in this document. The data were collected between April 2-20, 2023. A total of 1,311 cohort participants responded to the survey. Differences reported between groups are tested for statistical significance at a 95% confidence interval.
About ACS CAN
The American Cancer Society Cancer Action Network (ACS CAN) makes cancer a top priority for policymakers at every level of government. ACS CAN empowers volunteers across the country to make their voices heard to influence evidence-based public policy change that improves the lives of people with cancer and their families. We believe everyone should have a fair and just opportunity to prevent, find, treat, and survive cancer. Since 2001, as the American Cancer Society’s nonprofit, nonpartisan advocacy affiliate, ACS CAN has successfully advocated for billions of dollars in cancer research funding, expanded access to quality affordable health care, and advanced proven tobacco control measures. We’re more determined than ever to stand together with our volunteers to end cancer as we know it, for everyone. For more information, visit www.fightcancer.org.