Survivor Views: Affordability, Prescription Drugs, & Pain
Overview:
The American Cancer Society Cancer Action Network (ACS CAN) gives voice to cancer patients and survivors on critical public policy issues that affect their lives. As part of this effort, ACS CAN deploys surveys to better understand cancer patient and survivor experiences and perspectives, through our Survivor Views research panel. The panel is a group of cancer patients and survivors who respond to regular surveys and provide important insights to support ACS CAN’s public policy work at all levels of government.
Fielded October 22-November 19, 2021, the latest survey explores the affordability of health care for cancer patients and survivors, prescription drugs, and pain management. The web-based survey was conducted among 1,248 patients and survivors nationwide diagnosed with or treated for cancer in the last seven years.
Key Findings:
- A majority of cancer patients and survivors find it difficult to afford care, and 37% say it is difficult to pay for the prescription drugs and treatments associated with their care.
- Over 80% of cancer patients and survivors have taken steps to address their health care costs, with the plurality (44%) taking money out of savings to pay for their health care and 36% accumulating credit card debt to pay for health care expenses.
- Those most economically vulnerable face the greatest difficulty: Over half of lower income earners (55%) say prescription costs are difficult to afford and one-in-five (20%) say they are very difficult.
- Cost is a significant factor in treatment decisions for lower income cancer patients: 15% of those with annual household income under $35,000 say cost is the primary factor in making decisions about their treatment and care. One-third have cancelled or delayed an appointment or procedure because of cost and another third have delayed or not filled a prescription in order to reduce their costs.
- Cancer patients and survivors face treatment obstacles due to costs as well as coverage issues. Sixty percent have taken steps to reduce costs and nearly half have faced delays or difficulties accessing their prescribed medication or treatment for insurance-related reasons.
- Most cancer patients and survivors face pain that limits work, time with family, or social activities (59%); but they are only moderately satisfied with their pain management options. The main reason for dissatisfaction is that pain sufferers often don’t want to take an opioid pain medication but can’t find an effective alternative (44%). Thirty percent say their doctor has indicated that their options are limited by laws, guidelines, or coverage, but lower income earners report such limitations at a much higher rate. Fifty-five percent of cancer patients and survivors are worried about having access to adequate pain management in the future.
Detailed Survey Findings:
A Majority of Cancer Patients and Survivors Find it Difficult to Afford Care
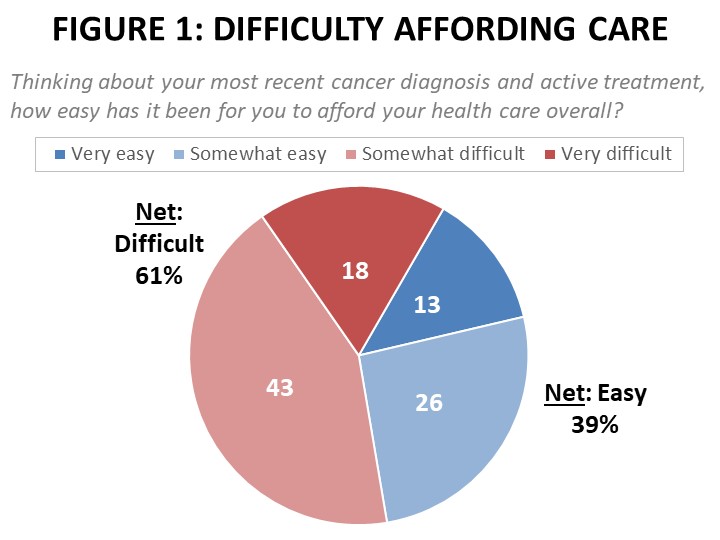
Sixty-one percent of cancer patients and survivors find it somewhat or very difficult to afford their care, and 37% say it is difficult to pay for the prescription drugs and treatments associated with their care. These findings are consistent with results from a February 2020 Survivor Views survey conducted shortly before the Covid-19 pandemic took hold in the US. Those enrolled in individual insurance plans and on Medicaid are more likely than those with employer coverage to report it’s been “very difficult” to afford their care. Half of those enrolled in Medicare say it has been difficult.
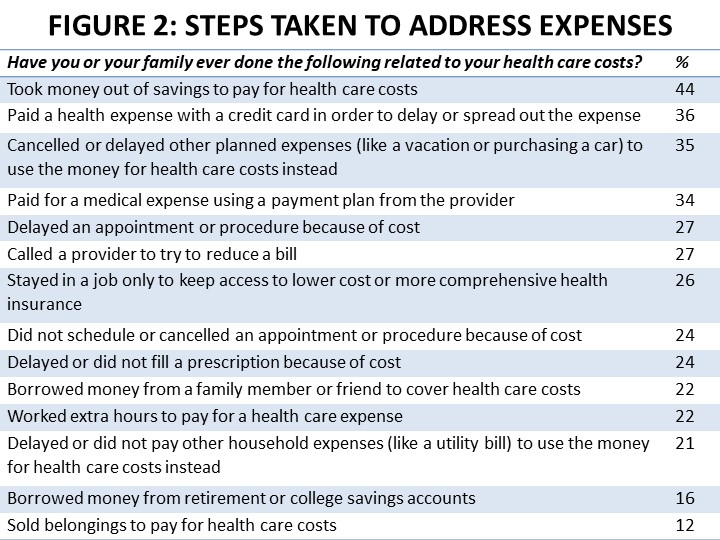
Over 80% of cancer patients and survivors have taken steps to address their health care expenses, with the plurality (44%) taking money out of savings to pay for their health care and 36% accumulating credit card debt to pay for health care costs. Over a third have cancelled or delayed other planned expenses in order to afford their care (35%), or utilized a provider’s payment plan (34%).
While 37% overall say it is difficult to afford the cost of prescription drugs and therapies, those most economically vulnerable face the greatest difficulty. Among lower income earners (those with annual household income of $35,000 or less), 55% say prescription costs are difficult to afford and one-in-five (20%) say they are very difficult. By comparison, 18% of higher income earners (those in households earning over $125,000 annually) find these costs difficult and only 4% say they are very difficult. Significant portions of patients across all insurance types report struggles with affording prescription drugs, including nearly 40% of those enrolled in Medicare.
Cost is a Significant Factor in Treatment Decisions for Lower Income Cancer Patients
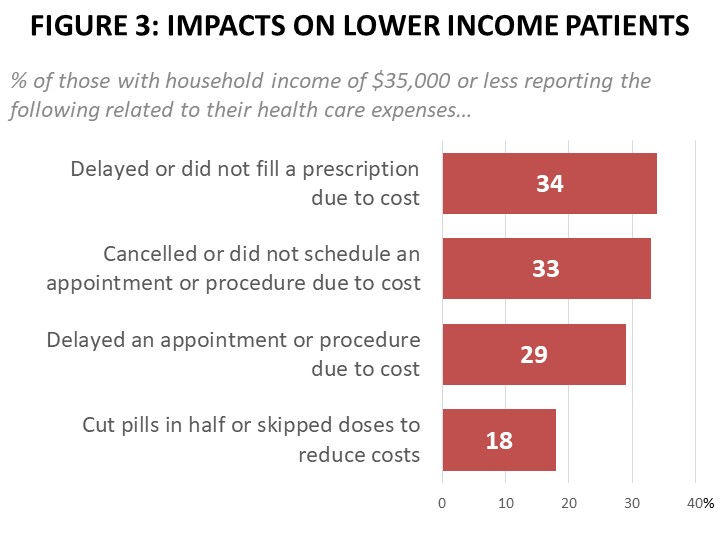 For more than half of those earning $70,000 or less, cost is one of if not the most important factor. Fifteen percent of those earning under $35,000 annually say cost is the primary factor in making decisions about their treatment and care. Additionally, one-third of lower income earners ($35,000 or less) report cancelling or not scheduling an appointment or procedure due to cost, and 29% have delayed an appointment or procedure due to cost. Those enrolled in privately-purchased plans (35%) and Medicaid enrollees (32%) are more likely to have cancelled or not scheduled an appointment, while those enrolled in employer-sponsored plans (24%) and Medicare (17%) are less likely to do so.
For more than half of those earning $70,000 or less, cost is one of if not the most important factor. Fifteen percent of those earning under $35,000 annually say cost is the primary factor in making decisions about their treatment and care. Additionally, one-third of lower income earners ($35,000 or less) report cancelling or not scheduling an appointment or procedure due to cost, and 29% have delayed an appointment or procedure due to cost. Those enrolled in privately-purchased plans (35%) and Medicaid enrollees (32%) are more likely to have cancelled or not scheduled an appointment, while those enrolled in employer-sponsored plans (24%) and Medicare (17%) are less likely to do so.
Furthermore, over one-third (34%) of lower income earners have delayed or not filled a prescription to reduce their costs, compared to 18% of those earning over $70,000 per year and 15% of higher income earners (over $125,000). This group is also disproportionately more likely to report having cut pills in half of skipped doses to reduce costs (18% of lower income earners have done this compared to 11% of the total sample and 5% of higher income earners). Medicaid recipients are most likely to report skipping or delaying a prescription in order to reduce costs (33%), compared to 28% enrolled in privately-purchased plans and 22% enrolled in Medicare. Women are twice as likely as men to report delaying or not filling a prescription to control costs (26% women, 13% men).
Cancer Patients and Survivors Face Treatment Obstacles Due to Costs as Well as Coverage Issues
Thirty-seven percent of patients and survivors overall find it difficult to afford their prescription drug costs, and 10% find it very difficult. While lower income cancer patients and survivors have been most impacted by prescription drug costs, 60% of all patients have taken steps to reduce their prescription drug costs. Chief among these are requesting generic drugs (35%), followed by using a drug manufacturer’s coupon or assistance program (28%), and asking a doctor to prescribe a less expensive medicine (20%). Seventeen percent of all patients have delayed or not filled a prescription due to drug costs, and 14% have endured a symptom without any prescription treatment. Ten percent have cut pills in half or skipped doses to reduce their medication costs.
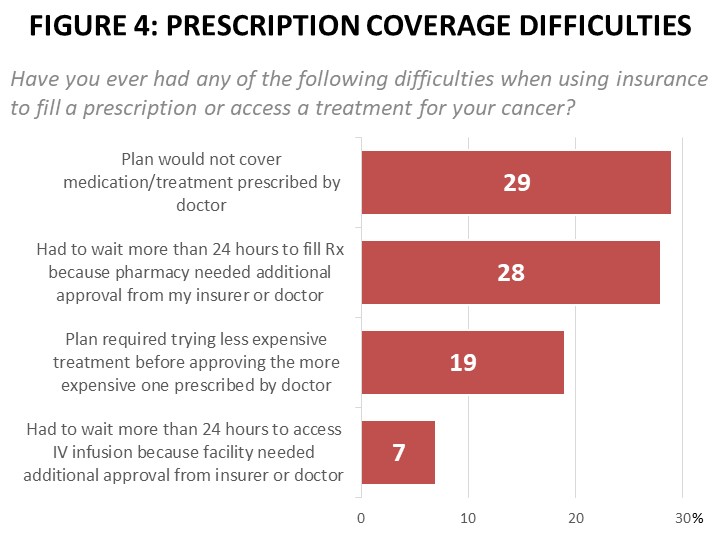 Nearly half (49%) have faced significant obstacles to filling prescriptions and accessing treatment. For instance, 29% have been told their plan would not cover a medication or treatment prescribed by their doctor. Among those enrolled in privately-purchased plans the impact is even greater – 40% of those enrolled in privately-purchased plans have been told their plan would not cover a prescribed medication. Another 19% have been required to try a less expensive medication or treatment before they were able to get the more expensive medication or treatment initially prescribed by their doctor.
Nearly half (49%) have faced significant obstacles to filling prescriptions and accessing treatment. For instance, 29% have been told their plan would not cover a medication or treatment prescribed by their doctor. Among those enrolled in privately-purchased plans the impact is even greater – 40% of those enrolled in privately-purchased plans have been told their plan would not cover a prescribed medication. Another 19% have been required to try a less expensive medication or treatment before they were able to get the more expensive medication or treatment initially prescribed by their doctor.
Seventy-nine percent report that prior authorization is required by their insurer for treatments and services such as diagnostic scans (59%), surgical procedures (37%), prescription drugs (31%), and radiation therapy (28%). Over a quarter (28%) have had to wait more than 24 hours to begin a medication while the pharmacy was awaiting approval. Seven percent have had to wait more than 24 hours to begin an IV infusion due to prior authorization delays. Delayed infusions are more commonly experienced by those enrolled in privately-purchased plans (10%). Most alarmingly, of those who had to wait more than 24 hours to begin an IV infusion, the plurality (45%) waited five days or more. For those waiting more than 24 hours for a prescription drug to be filled by a pharmacy, 26% waited five days or more, while 47% waited two to three days.
Twenty-eight percent of patients and survivors have had to make multiple calls to their pharmacy, insurer, or doctor to resolve difficulties with using their insurance to pay for prescriptions, and another 23% have resorted to paying for the medication out of pocket. Ten percent went without the medication for a week or more while resolving the issue. Those enrolled in privately-purchased plans were more likely to say they went without the medication or treatment for a week or more (18%), compared to 7% enrolled in employer-sponsored plans and 14% of those on Medicare.
With Only Moderate Satisfaction in Current Options, Room for Improvement in Pain Management
Fifty-nine percent of cancer patients and survivors experience pain that limits work, time with family, or social activities, but only 27% feel their options for managing the pain associated with their cancer meet their needs very well. The plurality, 44% say their pain management options meet their needs only somewhat well, and another 26% say their options do not meet their needs very well or at all. These findings are consistent across those treating their pain with non-opioid medications (comprising 58% of respondents), those taking an opioid (43%), those employing a non-medication treatment such as physical therapy (27%), and those not treating their pain at all (12%).
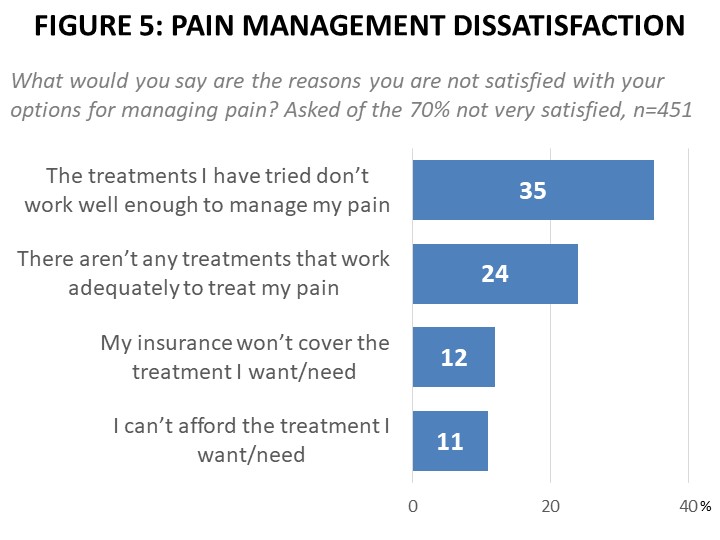
The primary reason for dissatisfaction with the options available for pain management comes from patients who don’t want to take an opioid pain medication but have not found an effective alternative (44%). Over one-third (35%) say the treatments they’ve tried don’t work well enough to manage their pain, and 24% say there are no effective treatments for their pain.
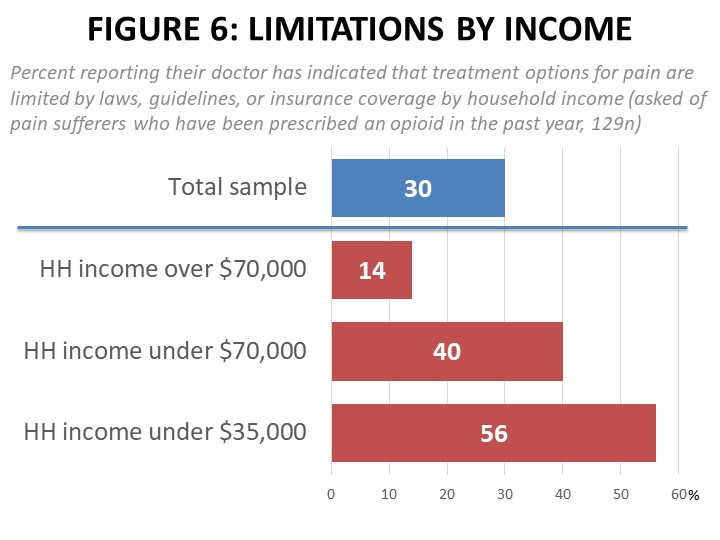
Among those who have been prescribed an opioid pain medication within the past year, 30% report that their doctor has indicated treatment options for their pain were limited by laws, guidelines, or their insurance coverage. Lower income earners are much more likely to report this, with 40% of those earning under $70,000 in annual household income and 56% of those under $35,000 per year saying their doctor has indicated such limitations, compared to just 14% of those in households earning over $70,000. Over three-quarters of Medicaid recipients report their doctor indicating these limitations (78%), and those enrolled in privately-purchased plans are also twice as likely as those on employer-provided 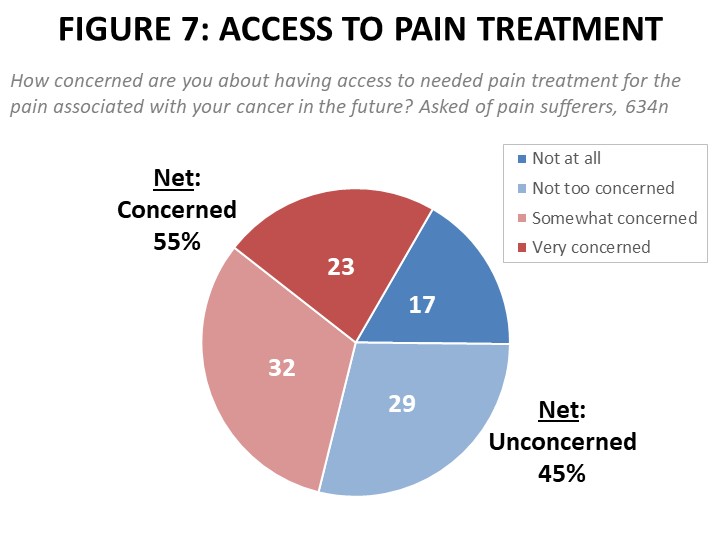 plans (40% vs. 20%) to say their doctor has indicated limits to their pain management options due to laws, guidelines, or coverage policies.
plans (40% vs. 20%) to say their doctor has indicated limits to their pain management options due to laws, guidelines, or coverage policies.
One-in-five report their pharmacy providing only a portion of the opioid medication written by their doctor (such as seven days instead of a prescribed thirty), and being told they had to call their doctor if more was needed. Another 20% say their doctor has informed them that prior authorization was required before they could prescribe a pain medication. Eleven percent said their insurance provider has required them to try an alternative pain medication before they could access the treatment prescribed by their doctor. Nearly half (47%) of those who have experienced difficulties filling an opioid pain prescription reduced their use of it regardless of their need for it, and 42% were unable to complete daily tasks or participate in work, family or social events due to uncontrolled pain. Fifty-five percent of cancer patients and survivors are concerned about having access to needed pain treatment for the pain associated with their cancer in the future.
Methodology:
ACS CAN’s Survivor Views research initiative was designed to enhance the organization’s mission to end suffering and death from cancer. Data provided by cancer patients and survivors as part of this project allows for a greater understanding of their experiences and opinions on cancer-related issues and gives voice to cancer patients and survivors in the shaping and advocating of public policies that help prevent, detect, and treat cancer and promote a more positive quality of life for those impacted.
To ensure the protection of all participants in this initiative all research protocols, questionnaires, and communications are reviewed by the Morehouse School of Medicine Institutional Review Board.
The survey population is comprised of individuals who meet the following criteria:
- Diagnosed with and/or treated for cancer within the last seven years
- Over the age of 18 (parents of childhood cancer survivors were invited to participate on behalf of their minor children)
- Reside in the US or US territories
Potential Survivor Views participants were invited to participate through email invitations, social media promotion, and partner group outreach. Those who agreed to participate after reviewing the informed consent information completed a brief survey including demographic and cancer history information to inform analysis as well as topical questions as discussed in this document. The data were collected between October 22 and November 19, 2021. A total of 1,248 participants responded to the survey, providing a margin of error +/-2.8 percentage points at a 96% confidence level.
About ACS CAN
The American Cancer Society Cancer Action Network (ACS CAN) is making cancer a top priority for public officials and candidates at the federal, state and local levels. ACS CAN empowers advocates across the country to make their voices heard and influence evidence-based public policy change as well as legislative and regulatory solutions that will reduce the cancer burden. As the American Cancer Society’s nonprofit, nonpartisan advocacy affiliate, ACS CAN is critical to the fight for a world without cancer. For more information, visit www.fightcancer.org.